Orthodontic appliances are generally divided into two major categories: removable orthodontic appliances and fixed orthodontic appliances. Fixed orthodontics is used to move and align teeth. This is while removable orthodontics is used to move the jaw. Fixed orthodontics is used to correct the distance between teeth and straighten crooked teeth. After diagnosing the type of abnormality, the orthodontist selects the best orthodontic tool for the patient orthodontic treatment program.
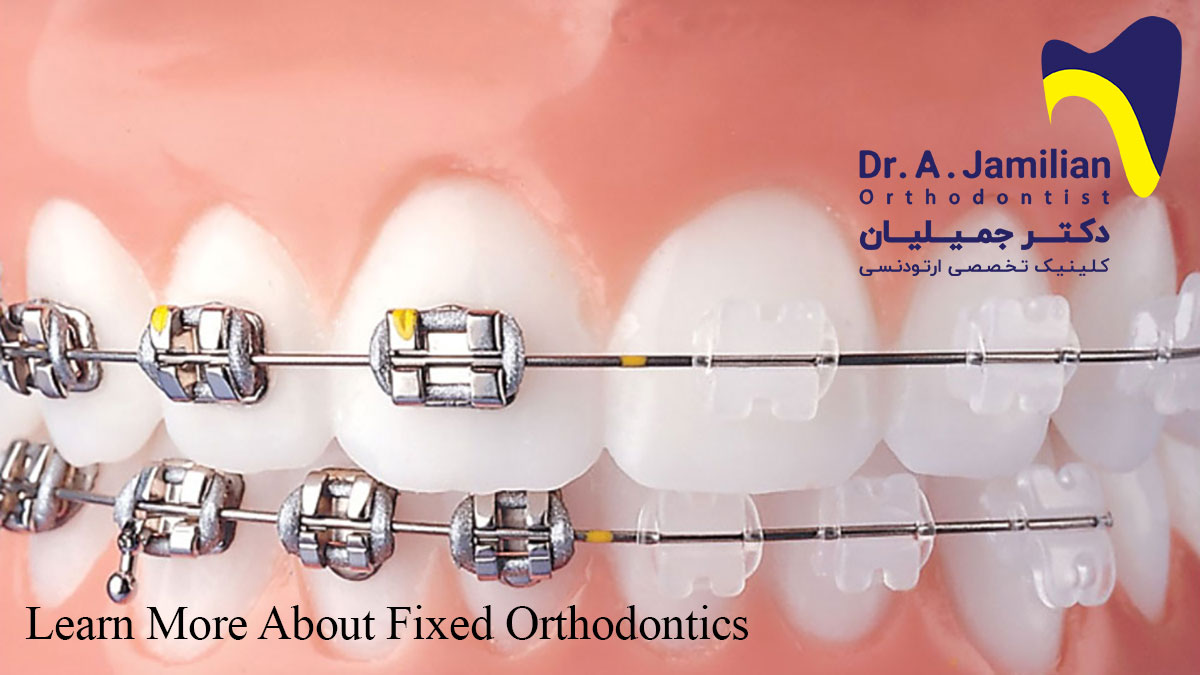
Fixed orthodontic appliances
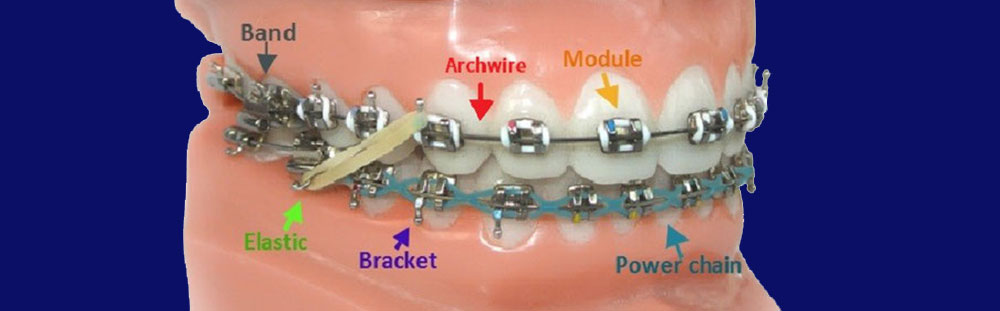
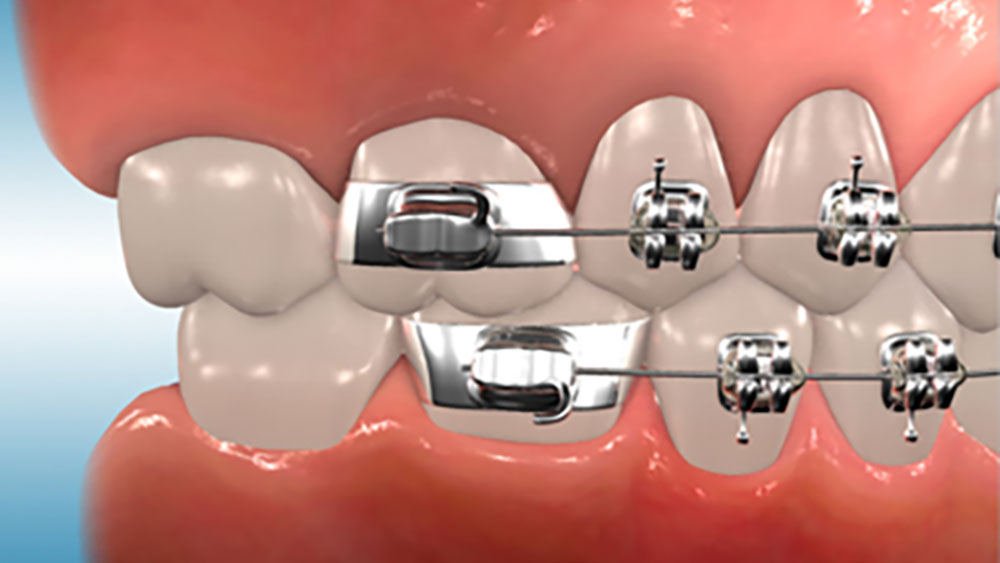
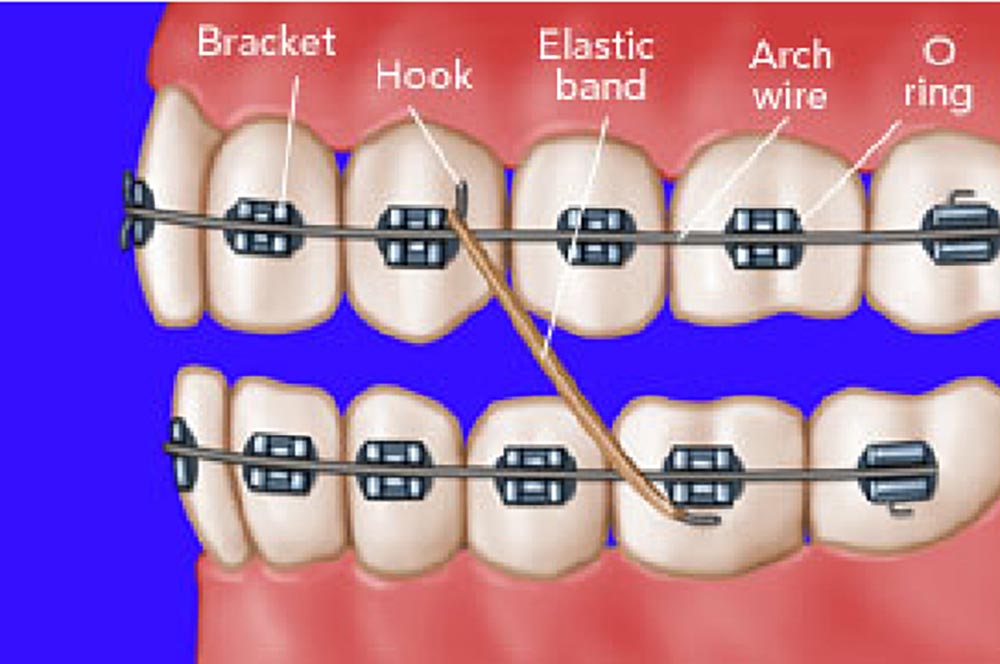
Common fixed orthodontic appliances have been generally developed based on the early edgewise appliance. The main components of a fixed orthodontic appliance are molar bands and brackets and its sub-components include headgear tubes, buccal tubes, buccal auxiliary hooks, lingual bottom, and auxiliary attachments. Molar bands are attached to teeth with cement, whereas brackets and other sub-components are either bonded or soldered to the band. The bands are placed on the first permanent molar or, in some cases, on the second permanent molar to enhance anchorage. The bands can be also used for anterior teeth, canines, and first and second premolars. However, the routine procedure in fixed orthodontics is to place the band on the first permanent molar.
The band is placed on the teeth with zinc phosphate, polycarboxylate, or glass ionomer cement, whereas other attachments are connected to teeth using composite material or to the band using cement. The replacement of gold bands with steel bands in orthodontics has made it possible to form steel bands around the teeth. The first prefabricated steel bands were those used for the anatomical filling of the crown in restorative dentistry. Prefabricated bands were abundantly marketed in the 1960s, and their different types with the right anatomical shape for each tooth are now available in the market.
Advantages of bonding in fixed orthodontics
Bonding the attachments directly to the tooth has undeniable benefits. Since these attachments have no interproximal tail, they are not necessary to be used for separated teeth. It is noteworthy that the teeth should be separated before placing the band. To this end, brass wires are put between teeth to increase the interproximal distance between them, so that they can be banded in the next session. Therefore, the direct bonding of attachments to teeth does not require tooth separation and, as a result, the patient will feel less pain. Compared to molar bands, the placement and removal of these attachments are easier and aesthetically better. In addition, it would be easier to use separation strips when there is a problem with the size of the bracketed tooth, because the proximal surfaces are free. The bonded attachments less irrigate the gums and reduce the risk of tooth decay and white spots. However, the brackets may also provide such benefits. Although the teeth are commonly bonded before the placement of attachments, there are cases where orthodontists prefer to use banding instead of bonding.
Banding is preferred to bonding in the following cases
1- Orthodontic treatments for teeth that are subject to intermittent-heavy forces: A good instance is the upper molars to which a headgear is to be attached. In such cases, bands can outperform bonds in bearing the shearing and twisting forces applied when placing and removing the headgear.
2- Orthodontic treatments for the teeth whose both labial and lingual surfaces should be connected to attachments, especially when the lingual attachment is not connected elsewhere: Although it is possible to bond the attachments to both the buccal and lingual surfaces of the tooth, it is easier both for the patient and the orthodontist to place a band with two attachments on the tooth. In addition, the banded attachments are less likely to be ripped off or swallowed.
3- Orthodontic treatments for teeth with a short clinical crown (SCC): In general, the edge of the band should be either slightly below the gums or at least 2 mm away from the gums in a way that the naked area can be cleaned. If the attachments (tube or bracket) are connected to the band, the band can slightly move the gums when it is in place. In contrast, bonded attachments can hardly do so. Depending on the length of the clinical crown of the tooth, the orthodontist decides to use either banding or bonding of the second premolars in adolescents.
4- Orthodontic treatments for teeth whose surface is not suitable for bonding: It is almost impossible to bond the attachments to the teeth whose surface is filled with amalgam or precious metal. Therefore, such teeth require banding for orthodontic treatments. Although it is difficult to bond attachments to porcelain restorations, this can be done by breaking the porcelain glaze and applying a coupling agent to improve the adhesion of the bonding material. Even under the highest bond strength, the connection between porcelain restorations and attachments will be weak and it will also extremely difficult to prepare some unrestored surfaces for bonding. For example, an early banding attempt is better than several unsuccessful bonding attempts in fluorosis cases.
Although there are always exceptions, attachment bonding for anterior teeth is almost always preferred in modern orthodontics. Depending on the length of the clinical crown and the need for lingual attachment, a band or a bracket is usually for premolars. In addition, attachment banding is usually preferred for molars, especially when both the buccal and lingual surfaces require attachments. It can be then concluded that modern orthodontics requires the use of prefabricated bands for premolars and molars. Anterior and canine teeth rarely need banding, except for cases where band material is used.
Separation in fixed orthodontics
The intense contacts between proximal surfaces of the teeth usually impede easy banding. It is hence necessary to somehow separate the teeth before banding. Although there are different types of separators, they do not follow the same principles in all cases. A separator is a device used to separate teeth from each other in order to stimulate the initial movement of the teeth and prepare them for banding in the next session. Separation may be a painful procedure, especially for anterior teeth, something which is considered a disadvantage of banding over bonding.
There are three basic ways to separate posterior teeth
1- Brass wire, A brass wire is tightly wrapped around the contact area of the teeth and stays in place for 5 to 7 days.
2- Spring tooth separator, This tool acts like scissors at the top and bottom of the contact area and usually provides enough space for banding within a week.
3- Elastomeric ring separator (donut separator), This tool is placed around the contact area of the tooth for 24 hours to contract and separates the teeth.
From patients’ perspective, spring tooth separators are the best option in terms of portability, easy placement and removal, and separation efficiency. The main drawback of these springs is that they may spontaneously loosen and be removed after they completely separate the teeth; that is why they are usually in place for only a few days.

Although it is more difficult to use brass wires or elastomeric ring separators, they remain firm in place for a longer time. Since elastomeric ring separators are radiolucent, they may pose serious problems if they are lost in the interproximal space. It is hence more logical to use color and radiopaque elastomeric rings that are more visible. Nevertheless, such separators should not be in place for more than two weeks.
It is possible to fabricate a band and connect the attachment to it in a dental clinic. However, it is more cost-effective for orthodontists to use prefabricated bands, especially in edgewise systems that require the placement of attachments at precise angles. This is because the accurate placement of attachments requires auxiliary tools. To fit a prefabricated band, we need to place the band on the tooth at maximum convexity. This allows the relatively soft band material to take the desired shape and harden simultaneously. It is then necessary to apply force and stretch to the band to completely encompass the tooth. This force should be taken from the patient’s masticatory muscles, not the dentist’s or their assistant’s hands and arms. The patients can apply this force in a more controlled manner by shutting their mouth and biting the band. However, some patients may be unable to shut their mouth and bite the band to apply the necessary force to direct the band to its right position.

Prefabricated bands are designed in a way that they should be placed and fitted according to the steps explained in the manufacturer instructions. For example, a typical maxillary band is designed in a way that should be first pressed against the mesial and distal surfaces until it reaches the bottom marginal edges and then be directed towards the mesiobuccal and distolingual corners. Finally, the patient should intensely bite the distolingual surface so that the band will be completely fitted. On the other hand, the lower molar bands are designed in a way that should be first pressed against the proximal surface and then be pushed down by applying heavy force to the buccal edge. The bands used for maxillary premolars can be completely fitted by applying alternate forces on the buccal and lingual edges, whereas the bands for the lower premolars are designed similar to the lower molars and can be placed on the tooth by only pressing them against the buccal edge. Due to the greater accessibility of the lingual surface, it is easier to fabricate a band for anterior teeth than posterior ones. This is now done in rare cases where dental bonding is not possible.
Orthodontic band cementation
Orthodontic band cementation is similar to cast restoration cementation, but there are differences between them in details. In restorative dentistry, most of the enamel is removed and the cement comes in contact with the dentin. By contrast, the cement completely covers the enamel in orthodontics. Zinc phosphate cement is still the best option for orthodontic treatments. Zinc phosphate cement is different from restorative cement in free phosphoric acid content. In fact, orthodontic cement contains more content of free phosphoric acid. The cement used for restorative purposes should be weak because the free acid can irritate the tooth pulp through open dentinal tubules, whereas the cement used in orthodontic treatments is relatively acidic in order to acid-etch the enamel (of course, not exactly like the de-bonding stage) and support the headgear. Additionally, orthodontic cement is thicker than inlay or crown cement, because the overflow of the extra cement from the band edges is not as problematic as cementing inlays or crowns and also a thicker mixture can provide further strength. It has been shown that glass ionomer cement outperforms zinc phosphate cement in molar bands. Glass ionomer cement can also release fluoride for several months, and if the cement breaks, it tends to stay on the tooth until it falls or comes in contact with the band. Both of these properties make the tooth resistant to decalcification. Slow setting time and difficult isolation are two major disadvantages of glass ionomer cement. Nevertheless, glass ionomer cement seems to be the best alternative for zinc phosphate cement in orthodontic band cementation. Regardless of the type of cement, the use of a cold slab can make it easier to cement several bands together. A cold slab also allows us to add more powder to the liquid and make a more rigid cement mixture. It is preferred to apply the frozen-slab technique for mixing cement powder.
Before placing the band. All internal surfaces of the tooth should be covered with the cement mixture in a way that there is no naked area on the teeth. Two types of archwires with different geometric properties are used in orthodontics: round archwires and rectangular archwires. The former only need bending before being used, whereas the latter requires both bending and torsion. Bending means to curve the archwire to rotate the tooth mesiodistally and torsion means to curve the archwire to rotate the tooth buccolingually. Removable orthodontic appliances can only use round archwires, whereas fixed orthodontic appliances can use both round and rectangular archwires. Rectangular archwires are usually used to rotate and move the tooth root. A fixed appliance can move or rotate the tooth root and a removable appliance can only tip the tooth crown. Therefore, when we need a bodily movement, we should use a rectangular archwire in a fixed orthodontic appliance.
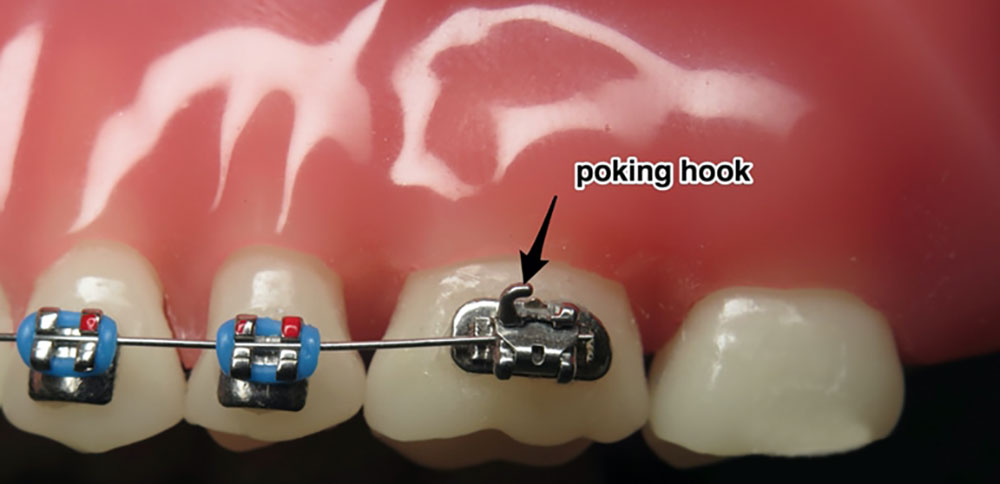
Another component of fixed orthodontic appliances is brackets. First, the tooth is etched with phosphoric acid for 1 minute and then let it dry. Then the surface of the tooth is covered with a layer of bond and composite material, and the bracket is placed on the composite material to attach to the tooth. The brackets are placed on the buccal surface of the posterior and anterior labial teeth. As the case may be, we can form the archwire in different shapes such as a circle or several loops. The archwire is connected to the bracket using an O-ring or a ligature wire. The placement and the removal of brackets are called bonding and de-bonding, respectively. In addition, the placement and the removal of the O-ring or band are called banding and de-banding, respectively. The molar band of the mandible usually includes a tube through which the archwire passes, whereas the molar band of the maxilla includes two tubes: one for the archwire and the other for the headgear. However, the molar band of the maxilla and the mandible may also include 3 and 2 tubes, respectively. An extra-oral appliance such as headgear includes an inner bow that is placed inside the molar band. A component of the inner bow that is located inside the molar band is called the headgear tube. A molar band also includes a hook that is connected to the elastic. Class-II elastics are used from the lower first molar to the upper canine tooth to correct Class-II malocclusions and Class-III elastics are used from the upper first molar to the lower canine tooth to correct Class-III malocclusions. Moreover, inter-maxillary elastics are used when elastics can go from the maxillary to the mandibular arch, whereas intra-maxillary elastics are elastics used in one arch only, either mandibular or maxillary.
Fixed orthodontic archwires
There are fixed orthodontic archwires of different grades. In the first stage of treatment, low-grade archwires are placed inside the bracket’s groove. Similar to twist archwires, low-grade archwires are highly flexible. Generally, low-grade archwires are more flexible than high-grade ones. Therefore, low-grade archwires are more appropriate for the first stage of treatment when the teeth are crowded. After this stage, the archwires of grade 12, 14, 16, 18, and 20 are used. In fact, as we approach the final stages of treatment, we use archwires of the higher grades. A 12-grade archwire, for example, refers to an archwire with a diameter of 0.012 inches.
One of the very first systems proposed for fixed orthodontics is the Begg system. The bracket groove is vertical (90-degree angle) in the Begg system, whereas it is horizontal in the Edgewise system.
A twist archwire is a flexible type of archwire usually used at the beginning of a fixed orthodontic treatment. Since the teeth are very crowded in the early stages of the treatment, we need to use a flexible archwire like twist archwire.
Why are low-grade archwires used in the early stages of fixed orthodontics?
What kind of archwires should be basically used:
1- Since archwires should exert light forces on crowded teeth in the early stages of the treatment, it is necessary to use low-grade archwires to achieve this goal.
2- The archwire should be able to freely move inside the bracket. A distance of 2 mm and 4 mm between the archwire and the bracket are considered necessary and favorable, respectively. Therefore, the 16-grade archwire is the thickest archwire that can be used in the 18-slot Edgewise system to move the teeth. In the 22-slot Edgewise system, the 20-grade archwire is the thickest archwire that can be used for this purpose but the 18-grade archwire is more favorable. It is once again noteworthy that 18-grade or 16-grade archwires, for example, refer to archwires with a diameter of 0.018 inches and 0.016 inches, respectively.
3- Rectangular archwires should not be used in the first stage of the treatment because they cause over-computability between the archwire and the bracket and also affect the position of the apex. During the initial alignment of the teeth, we only need to tip and move the crown and there is no need for the root displacement.

There are two systems of brackets:
018 (0.018 inches) and 022 (0.022 inches). These two figures refer to the height of the bracket groove. Some orthodontists work based on the 018 system and some others employ the 022 system. Orthodontists cannot constantly change the type of brackets they use.
The height of the bracket groove or, in other words, the occlusal-gingival distance in the bracket groove, is 0.022 inches in the 022 system and 0.018 inches in the 018 system. In addition, the groove depth in both systems is 0.028 inches. Therefore, the above-mentioned classification of brackets is based on the height of the bracket groove. When an orthodontist uses a low-diameter archwire in the 022 system at the beginning of the treatment, this archwire induces better movement in the 022 system compared to the 018 system. In other words, low-diameter archwires, such as 12-grade archwires, should be used in the first stage of the treatment. For example, a 12-grade archwire produces a clearance of about 6 mm in the 018 system and 10 mm in the 022 system. As a result, the tooth movement in the first stage of the treatment will be better in the 022 system. After correcting the crowded teeth, the archwires of higher grades can be used. The thickest archwires that can be used in the 018 and 022 systems are 16-grade archwire and 20-grade archwire, respectively. When a rectangular archwire is to be used in the final stage of treatment in the 022 system, it will become inflexible and stiff and cannot be easily fitted in the bracket due to its high diameter. By contrast, such archwires will be less stiff and inflexible in the 018 system and easily fits inside the bracket. Based on the advantages and disadvantages mentioned, orthodontists choose either of these two systems. The use of low-diameter archwires in the 022 system in the first stage of the treatment provides easier and better movement of the tooth, whereas the selection of the 018 system allows the orthodontist to more easily move and fit rectangular archwires inside the bracket. When orthodontists choose a system, they should always use the same system; since the archwire should be 2 mm smaller than the bracket groove, orthodontists should always be aware of the system they are working with in order to select and use the best archwires of different diameters.
There are generally two types of brackets: double or single; the former includes two pairs of wings and the latter has only one pair of wings. Double brackets are now more commonly used by orthodontists. The figure shows the back view of a bracket that is called mesh. The composite material sticks to this mesh behind the bracket and thus the bracket is bonded to the tooth. Brackets are usually made of ceramic, metal, or plastic, each of which has its own advantages and disadvantages.
Disadvantages of ceramic brackets in fixed orthodontics:
1- Since there is no computability between the archwire and the slot in ceramic brackets, there is high friction between them.
2- Since the bracket is placed on the buccal surface of the tooth, the bracket may sometimes interfere with the antagonist tooth due to occlusions. Therefore, this type of brackets can highly wear the antagonist tooth.
3- Ceramic brackets may damage the enamel when they are removed.
4- Drinking coffee or tea and smoking can discolor ceramic brackets.
5- Most patients desire to use less visible brackets. Like composite material, ceramic brackets may discolor over time. However, there is another system in which the brackets are bonded to the lingual surface of the tooth in order to obscure them.
6- Ceramic brackets are not recommended to be used for symptomatic teeth with signs of pathological pulp lesions or cracks on the enamel.
Metal brackets
Metal brackets are usually made of stainless steel:
and sometimes titanium, beta-titanium alloys, chrome, and cobalt. The main disadvantage of metal brackets is that they are visible and some patients are not willing to use them. Nickel allergy is one of the reasons for replacing metal brackets with ceramic ones. Since some patients insist that their brackets should be obscured, orthodontists may place metal brackets on the lingual surface of the teeth.
The disadvantages of placing brackets on the lingual surface of the teeth are as follows:
1- The main problem is the short inter-bracket distance.
2- Due to the low flexibility of lingual appliances, they need to be adjusted at short intervals.
3- Although it is possible to perform simple comprehensive treatments using lingual appliances, such treatments are more time-consuming and costly than treatments using labial appliances.
Plastic brackets:
The first-generation plastic brackets are made of polycarbonate and plastic molding powder.
Disadvantages of plastic brackets:
1- They can easily discolor if the patient is in the habit of drinking plenty of coffee and tea.
2- They are very fragile and may break over time. In other words, the slot is very fragile against the archwire.
The more recent generations of polycarbonate brackets include a metal slot and a plastic wing. In fact, all components of the bracket are made of plastic, except for the slot. The metal slot inside a ceramic bracket causes the archwire to be placed on and merge with the metal bed and reduces the friction between them. Recent ceramic brackets, which contain 15-30% filler, are stronger and less fragile.
Removable orthodontic palates
Removable palates are sometimes applied to expand the maxilla to allow dental movements. In fixed appliances, the band is placed on the first molar and premolar, and the miniscrew is activated twice in the first day (once in the morning and once in the afternoon) and only once in the following days, resulting in rapid palatal expansion. In this appliance, the suture opens and affects the maxilla base. The great forces applied to the molars and premolars lead to undermining resorption. If these teeth do not move at the buccal surface, these forces break the suture. In fact, constant forces are applied but do not move the teeth because the great forces applied to the buccal surface of the teeth have resulted in a destructive phenomenon called undermining resorption. This destructive process here beneficially impede the movement of teeth but breaks the suture groove and opens the palate.
If these teeth do not move at the buccal surface, these forces break the suture. In fact, constant forces are applied but do not move the teeth because the great forces applied to the buccal surface of the teeth have resulted in a destructive phenomenon called undermining resorption. This destructive process here beneficially impede the movement of teeth but breaks the suture groove and opens the palate.
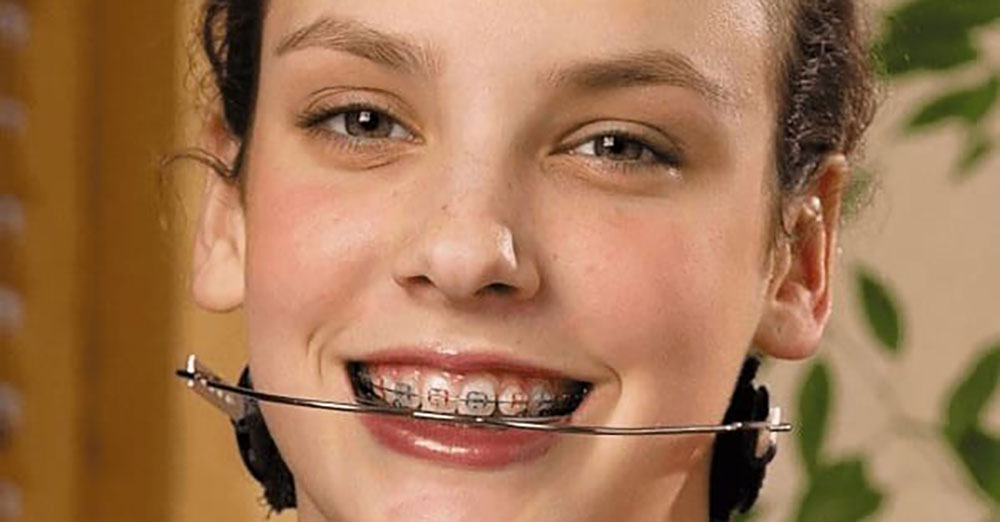
Orthodontic headgears
The molar is banded and then a headgear is placed on the band. The force is derived from the head or the neck and transmitted to the headgear and then to the tooth. Therefore, the type of headgear directs the movement of the molar. Cervical headgears or low-pull headgears are used to move the teeth distally. Since the distal movement of molars opens a bite, such headgears are appropriate for patients with deep bites. In other words, the further distal movement of the tooth leads to the development of a bite. If the headgear force or traction is derived from the neck, it is called a cervical headgear or a low-pull headgear, and if the force or traction is derived from the head, it is called an occipital headgear or a high-pull headgear. Since such headgears intrude the first maxillary molars, they can be appropriately used for patients with open bites.
We can have different maxillary rotations by changing the length of the outer bow and determining the place where the force passes through relative to the maxillary resistance center (either anterior maxillary resistance center or posterior maxillary resistance center). If the patient has a deep bite, we cannot use an occipital headgear because it may intrude the maxillary molars and exacerbate the condition. However, other factors are also involved in the selection of the best headgear, such as the patient’s profile and skeletal growth status. For example, when there is a vertical skeletal pattern or a horizontal skeletal pattern, we can use occipital headgears and low-pull headgears, respectively. When the headgear force or traction is derived from both the neck and head, it is called a combined headgear. Such headgears make the teeth bodily move backward.
Learn more about fixed orthodontics FAQ
The fixed orthodontic treatment duration depends on a variety of factors and may be different for each patient. The type of the patient’s orthodontics, the extent of damages to the teeth and jaw, the patient’s age and his/her physical condition are among the most important factors effective in specifying the orthodontic treatment duration. However, the fixed orthodontic treatment takes normally and averagely about 2 – 1.5 years.
Orthodontics is performed under the supervision of an orthodontist; if the patient feels any pain or discomfort during this process, he/she will use medications that can relieve the pain. Nevertheless, the pain caused by the fixed orthodontics is tolerable for most of the patients. After fixed orthodontic treatment, the patient may experience a little pain during their routine activities such as eating that will wear soon.
This cost may be different from each patient to another. Treatment costs depend on the factors including treatment duration, the equipment needed, patient’s condition and the tools used during treatment.
Yes, of course. However, fixed orthodontic treatment in adults might be somewhat more complicated than that in children. Adults may suffer gum diseases in addition to their jaw and tooth problems, which should be first cured under the supervision of a periodontist. On the other hand, the adults’ jaw and teeth bones are stronger than children’s; so they may need longer treatment duration.
The patient’s Jaw, teeth and gums are checked carefully by examining and using radiographic images to fully identify the damages. After thorough examination of teeth, the orthodontist guides the patient about probable problems of teeth through scaling, tooth extraction and prepares him/her for treatment. Formulating your treatment plan, the orthodontist can use the appropriate appliances required for your teeth.
Detachment of the bracket from the tooth means temporary cessation of the fixed orthodontic treatment. Since in fixed orthodontic treatment, the hardness and thickness of orthodontic wires are gradually increased, the brackets’ detachment will cause mouth ulcers or discomfort and slows down the treatment process.