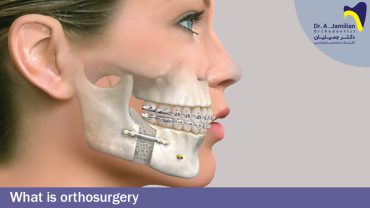
Some patients need both orthodontic treatments and surgical procedures. The patients with orthodontic problems who have undergone a growth spurt need a surgical procedure. For example, the protruded mandible of a 30-year-old patient cannot be corrected using a chincap. Another important point is heredity. When mandibular prognathism is inherited in a family, it cannot be treated only through orthodontic treatments. Such patients also need to undergo a surgical procedure. In addition, when the orthodontic problem is so severe, there will be no choice but to perform a surgical procedure to treat it. Less severe problems, especially those grouped under CI-III, can be treated using a chincap.
However, CI-III patients with a reverse overjet of 10 mm need both orthodontic and surgical treatments. The type of surgery depends on the type of malocclusion and facial profile. Orthodontic surgeries can be performed for individuals who have passed their growth ages, i.e. those aged over 17-18 years. Therefore, in the case of patients whose orthodontic problems are so severe that they cannot be corrected by growth modification or camouflage treatment, the only choice is to dislocate the jaws or part of the dentoalveolar structures. In such cases, surgical procedures cannot replace orthodontic treatments, but orthodontic or other dental treatments can provide conditions for the success of surgical procedures.
Mandibular prognathism was first treated by surgical procedures in the early 20th century. Dr. Edward Engel argues that orthodontic treatments and occlusal splint following a surgical procedure can produce the best therapeutic results for patients with orthodontic problems. The introduction of sagittal osteotomy by Obwegeser and Trainer in 1959 was considered a milestone in orthognathic surgery. This intraoral surgical procedure allows us to move the mandible backwards or forwards and also rotate it to correct the malocclusion.
Surgical procedures are performed when orthodontics alone cannot solve the problem. In addition, growth modification is applied when the patient is still within the growth period, and the orthodontist can take advantage of the growth potentials to correct the malocclusion. However, when the growth period is finished, the mandible can be easily moved backwards or forwards along the sagittal plane in a surgical procedure. The extra forward movement of the mandible in CI-III patients along the sagittal plane can reduce the therapeutic stability due to stretching the surrounding soft tissues and the disruption of neuromuscular adaptation.
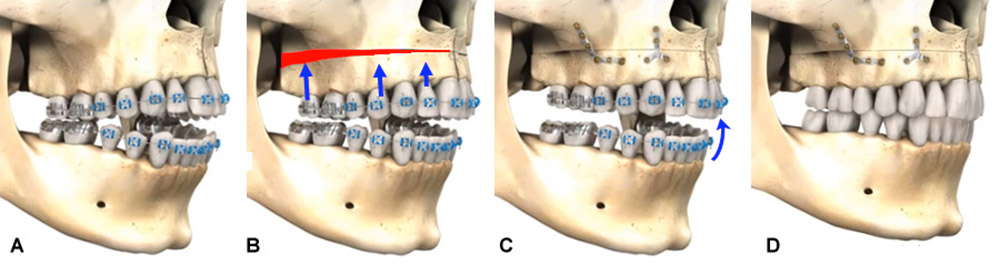
Maxillary surgery
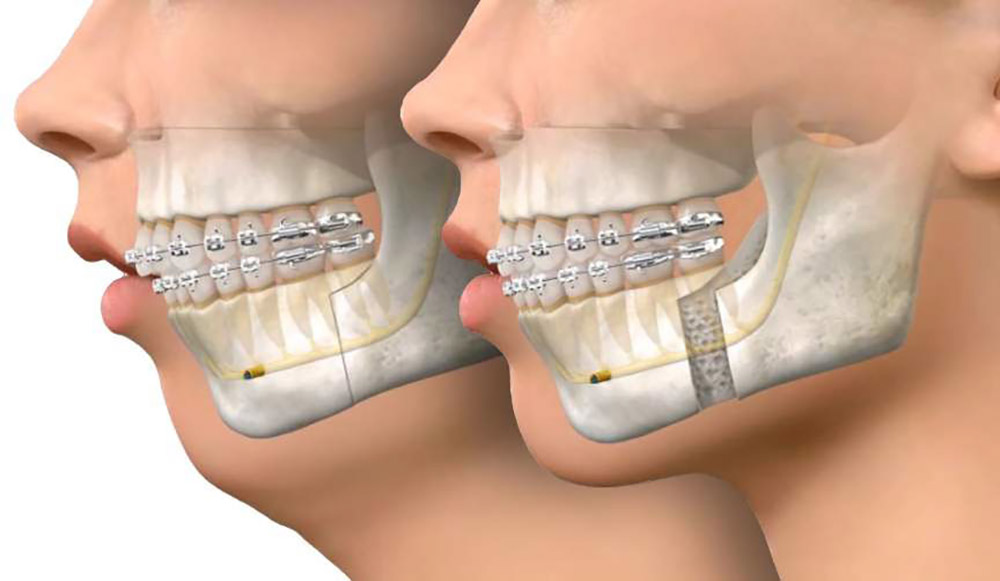
The maxilla can be moved forward by placing a graft in the posterior region to increase the treatment stability. However, it is not easy to move the whole maxilla posteriorly, because the bones that naturally encompass the maxilla interfere with its posterior movement. A solution to overcome this problem is maxilla segmentation, which allows us to move back only the anterior part of the maxilla. Down fracture is a technique that helps us to greatly move the maxilla forwards. Blood vessels and soft tissues are two major factors that restrict the surgical procedure. It is usually necessary to place a graft in the retromolar space. Different materials such as autogenous bone, dry-frozen bone, and alloplastic materials can be used as grafts.
Maxillary retraction is restricted by anatomical structures located near the pterygomaxillary fissure. Although the removal of bones from the maxillary tuberosity provides little space for movement, it is difficult to do so because both the area is not easily accessible and the surgical site is full of arteries. The more common procedure applied in such cases includes the extraction of premolars, maxilla segmentation, and placement of the anterior part inside the created space. The maxillary LeFort I osteotomy is the surgical procedure performed for the treatment of skeletal open bites. This procedure aims to elevate or, in other words, impact the posterior part of the maxilla to correct the open bite.
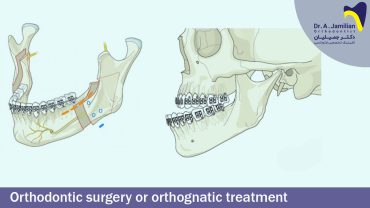
Mandibular surgery
Bilateral sagittal split osteotomy (BSSO) is currently the most preferred method for the treatment of patients who need mandibular extrusion. The introduction of this intraoral surgical technique fundamentally changed the procedure to reduce the detachment of levator muscles that contain the higher coils. These changes have increased the therapeutic stability and reduced tissue dissolution. This osteotomy technique provides a large, vascular bony surface for rapid healing of the area.
The overlapping of two bony segments allows easy fixation by intraosseous wiring or screw osteosynthesis. This prevents post-treatment instability. Internal fixation by using screw osteosynthesis is completely compatible with BSSO, adding to the popularity of this method among the mandibular extrusion procedures. One of the advantages of rigid fixation in BSSO is the excellent postoperative stability. Therefore, the patients can move their jaws and have their desired diet shortly after the surgery. In addition, this method shortens the duration of orthodontic treatments.

However, a disadvantage of BSSO is that the patient may face sensory changes and will be unable to open their mouth as much as before. Although it is common to cut the long buccal nerve to expose the surgical area, patients rarely complain of paresthesia of the tissues that feed on this effect. The sensory changes related to the lingual nerve are generally transient. The inferior alveolar nerve paresthesia almost always occurs immediately after the treatment but usually disappears after 2-6 months. Nevertheless, about 20-25% of patients may experience long-term sensory changes. It should be explained to patients that this negative effect has nothing to do with motor function. The hammering done to complete the sagittal detachment may cause the nerve to be compressed where it passes through the medullary bone.
The procedure to remove a neurovascular bundle to expose the adjacent osteotomy segment and then place it inside the movable part of the mandible may be damaging. Although slight maxillomandibular restrictions are common after such a surgical procedure, scientific data reveal that they are greater after BSSO than other methods. This may be attributed to the additional dissection of the mandibular midline. To recover the mandible’s normal range of motion, the patient must follow a physiotherapy regimen after the surgery. Orthopedic studies have proven the effectiveness of inactive continuous movements for this purpose. There are two other methods for mandibular extrusion. One of these two that attracted less attention is the inverted L-osteotomy. In this intraoral surgical procedure, it will be very difficult to achieve postoperative stability without using a graft because the bone contact surface is limited. Another method is c-osteotomy and its derivatives that are usually performed as extraoral procedures.
In mandibular advancement surgery, it is better to fill the spaces created by the jaw extrusion with grafts to increase the treatment stability and prevent window defects. The mandibular advancement surgery is usually performed for patients who cannot undergo intraoral procedures due to the limited accessibility resulting from their pathological conditions. Subapical surgery makes it possible to extrude both the alveolar processes and teeth. This surgery is performed for patients whose chins are sufficiently protruded but their dentoalveolar structure distally moves on the trunk of the jaw.
The extent to which the mandible can be extruded depends on the dimensions of the dentoalveolar structure. Such sagittal problems are usually accompanied by a vertical deficiency, which can be corrected by placing a bone graft under the alveolar segment. Although subapical surgery requires the detachment and displacement of the mandibular nerve bundle, it is not more likely than BSSO to cause sensory problems. Mandibular retraction is also done by BSSO, a method that is commonly applied to move the mandible both anteriorly and posteriorly. BSSO is widely used for mandibular retraction because it both provides excellent control over the condylar segment and makes it possible to use screw osteosynthesis.
Another method for mandibular retraction is transoral vertical ramus osteotomy (TOVRO). This technique, which is merely performed for mandibular retraction, requires the full overlapping of the two cut segments. This technique was initially performed extraorally, but the technological improvement of surgical instruments has made it possible to perform this surgery as an intraoral procedure. This surgical procedure takes less time and is less likely to cause sensory changes. However, the limited visibility and accessibility during the surgery impede any type of internal fixation. Therefore, maxillomandibular fixation is usually done after TOVRO. It has been experimentally shown that the mandible can begin functioning in a controlled manner 7 to 10 days after surgery if special elastics are used to guide the mandible.
A complete orthosurgery procedure typically includes the following stages:
- Preoperative orthodontics
- Surgery
- Postoperative orthodontics
- Prosthetic treatments
The preparative orthodontics includes the following stages:
- De-crowding, alignment, and leveling
- Arch decompensation
- Arch coordination
Leveling is the process in which the incisal edges of the anterior teeth and the buccal cusps of the posterior teeth are placed on the same horizontal level, alignment refers to the lining up of teeth of an arch in order to achieve normal contact point relationships, and de-crowding means to arrange the teeth in a regular manner. Arch decompensation, which will be explained later, refers to correcting the compensated teeth. Finally, arch coordination aims to match the two dental arches in order to achieve postoperative occlusion.
Orthosurgery procedure
For all patients undergoing an orthosurgery, the type of surgery should be determined: maxillary extrusion or retraction, mandibular extrusion, retraction, rotation, impaction, and maxillary widening or narrowing. The opposite is true for Cl III patients who have a small and retracted mandible and their lower incisors always tend to approach the labial surface. In other words, the mandible naturally tends to move forwards but only the incisors can move forwards because the whole mandible is retracted. Therefore, in CI-III patients whose mandibular incisors tend to approach the labial surface, it is necessary to take preoperative orthodontic treatments to move the mandibular incisors toward the lingual surface to place the teeth on a healthy base.
The teeth should be further overjeted to provide more space for mandibular extrusion. In fact, the compensated mandibular incisors of CI-III patients that are inclined towards the labial surface should be decompensated. The patient’s jaws are molded to be sent to the surgeon to choose the best surgical procedure based on the type of malocclusion.
Therefore, the patients who need orthosurgery should undergo first orthodontic treatments, which are different from ordinary orthodontics, and then main surgery. However, the orthodontic treatments may continue for 6 months to 1 year after the surgery. Some patients who miss some of their teeth (e.g. lateral teeth) may need to receive prosthetic treatments, such as the placement of a pontic. Some cases may also require nose surgery. Therefore, an orthosurgery team consists of anorthodontist, a prosthetist, and a maxillofacial surgeon.
Before an orthosurgery, it is necessary to first align and level the patient’s teeth. Leveling is the process in which the incisal edges of the anterior teeth and the buccal cusps of the posterior teeth are placed on the same horizontal level. In fact, the teeth should not be intruded or extruded irregularly. If the patient has crowded teeth, there may be a need for extracting some of the teeth. Therefore, the first step of orthosurgery is dental aligning, leveling, and de-crowding. The next step is dental decompensation, that is to say, for example, to procline the mandibular teeth of a Cl-III patient that have been naturally ligualized. In fact, dental decompensation aims to return the incisors to their normal position before the surgery.
In some cases where arch decompensation is not performed, the surgeon will lose the necessary maneuvering power in the operating room and the surgeon and the orthodontist will be confused about the surgical procedure. In CI-III patients who do not need to undergo surgery, the anterior teeth of the mandible should be aligned lingually or, in other words, the mandibular incisors and the entire mandible should be retracted.
The next step is to coordinate the upper and lower arches. Therefore, the surgery is performed after dental aligning, leveling, de-crowding, decompensation, and coordination. The first step after surgery is intermaxillary fixation (IMF). To this end, the mandible and the maxilla are attached for 8 weeks and the patient should eat only by using a straw. If the connection is provided by screws and plates, not wires, it is called rigid fixation.
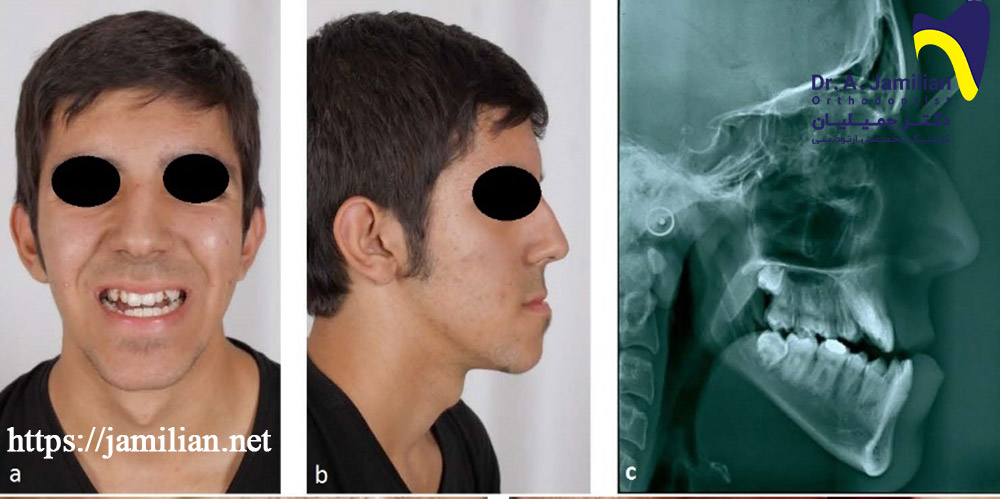
The following slide is related to a patient who was treated based on a wrong orthodontics plan, whereas the patient should have undergone orthosurgery. The patient is dissatisfied with the height of the face and suffers from lip incompetence, i.e. the lips are open more than 3-4 mm at rest; the patient feels a sense of stretch when closes the lips, and the mandible is retracted. The previous dentist had flared the upper and lower teeth to bring the lips together. However, the patient is not happy with the facial profile and the retracted mandible. Therefore, we need to intensify the CI-II conditions by further overjeting the first 2 mandibular premolars. Since the maxilla is not much extruded in this patient, we can extract the second premolars of the maxilla to reduce their effect on the maxillary profile. Therefore, 2 units of the maxilla (second maxillary premolars) and 2 units of the mandible (first mandibular premolars) were extracted in the patient.
In this patient, the first premolars of the mandible were extracted to further overjet the patient and the second premolars of the maxilla were extracted to slightly correct the maxillary crowded teeth. After coordinating the mandible and the maxilla through fixed orthodontics, the mandible was extruded in a surgical procedure to correct the retraction caused by mandibular deficiency.
It can be hence concluded that different treatments should be planned for patients who need only orthodontics and those who need both orthodontics and orthosurgery. This necessitates determining from the beginning whether or not the patient needs surgery. The orthosurgery may generally involve maxillary retraction, advancement, and impaction or moving the maxilla downwards. Other possible options include mandibular advancement and mandibular setback. Postoperative orthodontics also involves dental aligning and leveling. Since some teeth may move out of the dental arch or rotate due to the fracture of the dental wires, it is necessary to perform orthodontic treatments to align and level the teeth. If the surgical procedure makes changes in the dental arches, the postoperative orthodontics should also involve arch coordination. After removing the wires, the patient is prescribed to use a retainer depending on the type of malocclusion.
It may be necessary to extract some teeth in patients undergoing orthosurgery. The extraction pattern includes the maxillary first premolars and the mandibular second premolars for CI-III patients undergoing mandibular setback and the maxillary second premolars and the mandibular first premolars for CI-II patients undergoing mandibular advancement. In patients that need to merely undergo orthodontics, the pattern of the possible extraction includes the maxillary second premolars and the mandibular first premolars for CI-III patients and the maxillary first premolars and the mandibular second premolars for CI-II patients.
However, the above-mentioned patterns may change based on other factors such as facial profile, tooth decay, and the existence of open bites or deep bites. Since there are different extraction patterns for patients undergoing orthosurgery or those who only need orthodontics, the treatment plan should be determined from the beginning (orthosurgery or orthodontics alone).