Tooth movement by orthodontic force application is dependent on remodeling in periodontal ligament and alveolar bone, involving the activation of complex cellular and molecular mechanisms correlated with several macro – and microscopic biological changes. The orthodontic process involves the activation of many complex cellular and molecular mechanisms mediated by the release of chemical substance cascades by many cells of the periodontium.

Mainly during the early stage of application of orthodontic forces, an inflammatory process can occur in the periodontium as a physiological response to the tissue stress. Several potential biomarkers of the biological alterations after an orthodontic force application expressing bone resorption and formation, periodontal ligament changes, and vascular and neural responses, may be detected. The appropriate choice of the mechanical force to achieve the highest rate of tooth movement in the shortest time of treatment avoiding adverse consequences is a primary objective of a specialist. Thus, an insight into the biological phenomena occurring during the orthodontic therapies by evaluating these biomarkers may be quite relevant for the clinicians. In this chapter, two models of study, i.e., mice and men, were used to describe the clinical usefulness of some biomarkers in orthodontics.
Introduction
Tooth movement by orthodontic force application is dependent on remodeling in periodontal ligament (PDL) and alveolar bone, correlated with several macro- and microscopic biological changes.
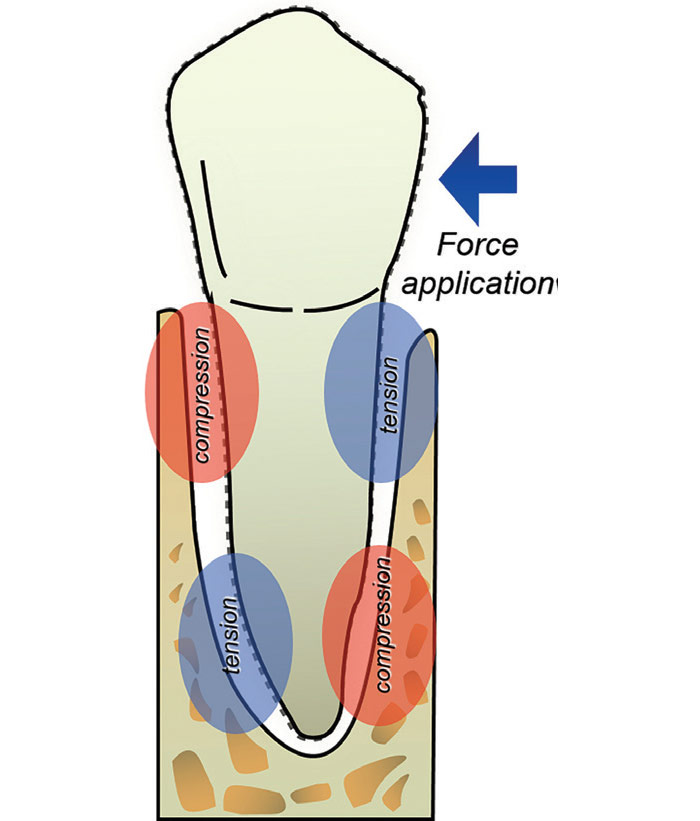
After more than 100 years, since the first article on the theory of tooth movement was published by Carl Sandstedt (1904–1905), the specialists have reasonably good understanding of the sequence of events involved in the orthodontic tooth movement at tissue and cellular levels [1]. Orthodontic movements represent a continual and balanced process characterized by bone deposition in tension sites and bone resorption in the pressure ones. The mechanical stress from the application of orthodontic forces induces the activation of many cellular and molecular mechanisms mediated by the release of chemical substance cascade allowing the transmission of signals from extracellular matrix. These alterations lead to a gradual remodeling of the mineralized (alveolar bone) and nonmineralized (periodontium) tooth supporting tissues during the orthodontic movement.
Mainly during the early stage of application of orthodontic forces, an inflammatory process can occur in the periodontium as a physiological response to the tissue stress. Several potential biomarkers of the biological alterations after an orthodontic force application may be detected, specifically expressing bone resorption and formation, periodontal ligament changes, and vascular and neural responses.
The appropriate choice of the mechanical force to induce the highest rate of tooth movement in the shortest period of treatment avoiding adverse consequences is a primary objective of a specialist. To identify the degree of remodeling occurring in the periodontal tissues during an orthodontic treatment by monitoring the levels of certain biochemical mediators may be a clinically useful procedure.
In this chapter, the importance of evaluating the levels of substances as valid biomarkers of periodontal effects of an orthodontic treatment is emphasized through a description of the specific role of each of them. Only studies on mice and rats have been considered as animal models, whereas in order to monitor the expression of these biomarkers noninvasively in humans, changes in the composition of gingival crevicular fluid (GCF) during orthodontic and orthopedic tooth movement have been selected as first choice. Substances involved in bone remodeling are produced by periodontal ligament cells in sufficient quantities to diffuse into the gingival crevicular fluid. Thus, by means of two different study models “mice and men,” the clinical usefulness of some biomarkers in orthodontics is properly analyzed.
2. Anatomy and function of periodontal ligament and alveolar bone
“Periodontium” comes from the Greek “what is around the tooth.” It includes all structures that anchor the tooth to the alveolar bone surrounding forming a strong support structure . Its components are gingiva, periodontal ligament, cement, and alveolar bone (Figure 1). The periodontal ligament is the structure interposed between the tooth root and the alveolar bone, with an area of 0.25–0.5 mm. It is a connective tissue whose main component is represented by a set of elastic collagen fibers, parallel to each other, inserted on one side in the cementum and on the other in the lamina dura of the alveolar bone (Sharpey’s fibers). The oblique direction of these supporting fibers on the tooth surface provides the tooth with enough elasticity to distribute the masticatory forces over a large surface of the alveolar process, allowing the