Gum and jaw recession is the process where the margin of the gum tissue surrounding the teeth wears away or pulls back. Jaw recession also occurs when the tissue of the jaw bone is pulled back or worn away. During the incident of gum recession, some cracks or gaps are developed between the teeth and the gum line, accelerating the accumulation of pathogenic bacteria. Failure to treat gum recession will injure the tissue and bone structure of the jaw and teeth (e.g., tooth root) and the patient may ultimately have his or her teeth lost.
Gum and jaw recession is a prevalent medical condition. Most patients know nothing about the underlying cause of this problem because the disease happens and proceeds gradually. The first serious sign of gum and jaw recession is dental hypersensitivity. The patient may also know that he or she has a tooth taller than normal.

Commonly, patients with gum and jaw recession feel a gap near the gum line. As a reminder, gum and jaw recession should be considered seriously. If you think your gums are pulling back, call your dentist.
Who is most likely to get gum recession?
Some factors can cause gum and even jaw recession, the following is a list of the most likely:
- Periodontal disease: Bacterial infections at the gum tissues cause the gum tissue & bone supporting the teeth to wear away. This condition is ultimately associated with the loosening of the teeth.
- Gum disease: Some patients may be genetically prone to a variety of gum diseases. Studies show that 30% of people may be genetically prone to this type of disease.
- Aggressive tooth brushing (over-brushing): When you are brushing with too much pressure or fast, this can damage the enamel and pull the gums back.
- Deficient care of teeth and dental plaque: Dental plaque is the accumulation of hardened microorganisms on the surface of teeth, which can lead to jaw and gum recession. Regular flossing and rinsing with an antibacterial mouthwash will eliminate plaque on the teeth.
- Variations and fluctuations in female hormones: Puberty, pregnancy, and menopause can make the gums more sensitive and prone to recession.
- Tooth cavity and latent teeth: In cases of severe tooth cavity, the patient may also suffer from gum recession and subsequent jaw resorption. When the patient has one or more latent teeth, food is in direct contact with the gum tissue, which leads to gum and jaw recession in the long run.
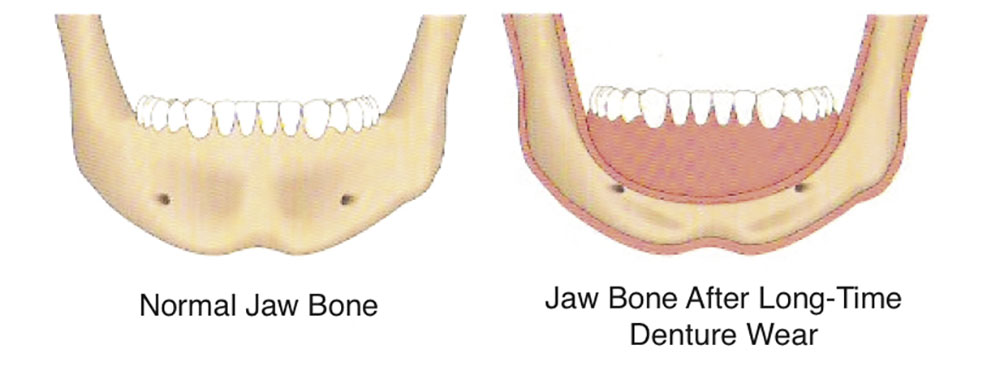
How does the jaw bone wear away?
Note that the gum tissue recession occurs prior to jaw bone recession. Jaw bone normally wears away gradually due to the loss of one or more teeth. In other scenarios, it often will occur when foods are in direct contact with the gum tissues. Dentures can also lead to jaw bone recession in the long run.
It is hundred-percent possible to avoid jaw bone recession by observing oral hygiene and proper dental care. If you have a lost tooth or are suffering from a latent tooth condition, make sure to see an experienced orthodontist for treatment to avoid the incidence of jaw bone recession.
How can we prevent a gum recession?
The best way to prevent gum recession is to take good care of your mouth and teeth. Brush and floss your teeth daily and visit your dentist minimally twice a year. Always use a toothbrush with a proper brush and ask your dentist or health care professional to train you how to brush correctly. If gum and jaw recession is due to a tooth cavity, then talk to your dentist about how to fix the problem. Other ways to avoid gum and jaw recession include the following:
- Smoking cessation
- A balanced and healthy diet
- Control over mouth variations
How is gum and jaw recession treated?
Gum recession can be treated and ended in the early stages with dental plaque and tartar removal. In this procedure, built-up plaque and tartar on the surface of teeth and below the gum line is carefully removed.
Open flap plaque and tartar removal and scaling and root planing are further prescribed in the treatment of gum and jaw recession. In this procedure, the dentist or a surgeon removes the damaged gum tissue surgically and eliminates harmful bacteria from the dental gaps, and then fixes the gum tissue to the dental roots firmly.
Bone grafting to treat jaw bone recession
If the bone supporting the teeth has been lost due to gum recession, then a procedure may be advised to restore the lost bone and tissue. First, the gum area undergoes flap surgery. A regenerative agent (e.g., a membrane, connective tissue, or tissue-stimulating protein) is then used to stimulate stem cells to regenerate the jawbone naturally.
How does jaw bone grafting preserve the gums?
The tooth cavity is first filled with a gelatinous agent and then its surface is covered. The gelatin sponge strengthens the bone material beneath it and regenerates the gum tissue. On average, the aforementioned procedure prevents 90% of bone and gum recession. In this technique, the patient receives his or her ideal implant with appropriate dimensions after 10 weeks, and in most cases, he or she no longer needs tissue reconstruction techniques.
Gum transplant and denture
A complication with using dentures is gum and jaw recession. Together with the jaw bone recession, the denture will no longer work efficiently and will not remain fixed. Therefore, the patient may be advised to undergo jaw bone grafting, not gum grafting. When jaw bone grafting is successful and the bone strip is fixed firmly, then the patient can use dental implants instead of dentures. However, when the jawbone strip is still not fixed enough for an implant, the patient will be advised to reuse the denture. In such cases, the former denture is no longer effective and the patient needs to purchase a new one.
Gum analysis following implantation
Gum recession following dental implants may happen in the short or long term. If the patient fails to observe oral hygiene necessities, gum recession will occur in the long run. Likewise, if the patient is anatomically sensitive to the implant, i.e., under transplant rejection, he or she will suffer from gum recession in the short term after the implant. In 95% of cases, the implant is successful and the patient will experience no sensitivity or reaction to this foreign material. In some cases, however, damage to the gingival nerves and arteries during implant exacerbates the complication of gum recession.
Gum and jaw recession FAQ
1-Should antibiotics be prescribed to treat gum and jaw recession?
The dentist may prescribe some antibiotics upon scaling in order to kill any harmful bacteria left behind. The type of antibiotics is determined (and then prescribed) by a gynecologist in acute conditions.
2-When is surgery advised to treat gum and jaw recession?
When the bone of teeth is severely damaged and there are deep gaps, gum and jaw surgery may be obliged to repair the damage caused by gum and jaw recession.
3-What surgical procedures are advised to treat gum and jaw recession?
Several types of gum tissue and jaw bone transplants are available to treat gum and jaw recession. However, connective tissue grafting is a widely established procedure.
4-What are the complications of bone grafting to treat gum and jaw recession?
Pain, swelling, bleeding, tooth sensitivity, and tooth root cavity are some complications of bone grafting in the treatment of gum and jaw recession.
5-How long does it take for a jaw bone graft to heal?
It depends on the patient’s physical status and health. Full recovery following a jawbone grafting may take about 4 to 9 months.
6-What to do following bone grafting to treat gum and jaw recession?
Avoid touching the wound, over-washing the mouth, and smoking. Having a good diet rich in vitamins can aid wounds to heal faster and diminish the convalescence it takes for a bone graft to restore.
7-Are dentures proper for gum worn away?
The patient may suffer gum and jaw recession, in addition to losing one or more of his or her teeth. Such patients usually have no good jawbone and cannot use dental implants. Therefore, using dentures is the only way to replace lost teeth in these patients.